The male and female reproductive systems differ in many ways. However, they also share some similarities. In both males and females, the most important organs for reproduction are the gonads (or primary sex organs). These are the testes in males and the ovaries in females. The male reproductive system being outside of the body is more obvious than that of the female reproductive system. However, there are internal and external structures.
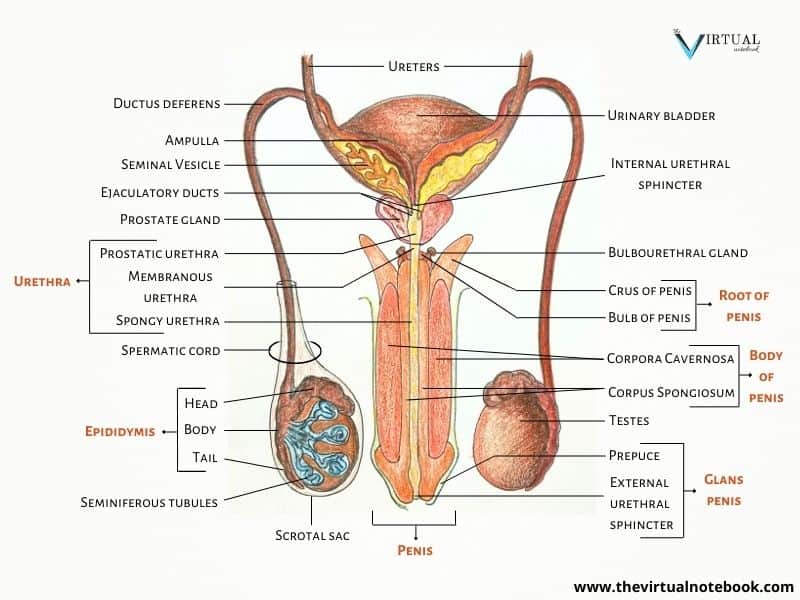
The external genitalia includes the penis and the scrotum. Meanwhile, the internal organs include:
- The testes, which contains sperms that pass through the duct system.
- The duct system, which comprises:
- The epididymis,
- Vas deferens (or ductus deferens),
- Ejaculatory duct, and
- The urethra.
- At last, the accessory glands, which secrete fluids that build up semen. These glands consist of:
- The seminal vesicles,
- The prostate gland, and,
- The bulbourethral glands.
Male reproductive system labelled diagram
Functions of the male reproductive system
The primary function of the male reproductive system is to accomplish reproduction. There are many other functions that make it possible. They are as follows:
- Production and secretion of male sex hormones.
- Lubrication of both male and female sex organs.
- Production, nourishment, and transportation of sperm, and
- To discharge sperm into the female reproductive tract.
Parts of the male reproductive system
Male external genitalia
1. Penis
The penis is the male organ of reproduction. It is flaccid for non-sexual actions, such as urination and rigid with sexual arousal. When erect, the stiffness of the organ allows it to penetrate the vagina and deposit semen into the female reproductive tract.
The penis has a root and a shaft. Markedly, the root anchors the penis in the perineum (the area between the anus and the genitals). In contrast, the shaft (body) is the externally visible, moveable portion of the organ. At its tip, there is a triangular structure, the glans penis. This is where the external urethral orifice is located. Just above the glans, the skin folds upon itself and forms a movable double layer, the foreskin (or prepuce). The foreskin is sometimes surgically removed by a common procedure known as circumcision.
As shown in the figure, three column-like bodies of erectile tissue span the length of the shaft. Each erectile body is a spongy network of connective tissue and smooth muscle filled with vascular spaces. The two lateral columns are the corpora cavernosa. On the other hand, the column between them containing the urethra is the corpus spongiosum. During sexual arousal, the vascular spaces fill with blood, which causes the penis to enlarge and become rigid.
2. Scrotum
Location
The scrotum is located between the thighs and behind the penis. This location helps in the production of sperms by maintaining optimal temperature. But how?
Under normal circumstances, the temperature of the scrotum is about 3° C lower than that of the core. The core body temperature of 37° C is too warm for the production of viable sperms. In like manner, too low a temperature can also impact spermatogenesis. (we will read about this in a later post)
In cold weather (or in water), the testes move upward to the warmth of the body wall. At this point, the scrotum becomes shorter and heavily wrinkled. In turn, it decreases the surface area of the scrotum and reduces heat loss. On the other hand, as the nearby temperature increases, the scrotum relaxes and becomes limp or soft. This increases the surface area for cooling (which may involve sweating) and moves the testes farther away from the warmth of the body. This, in turn, promotes heat loss. By all means, two distinct muscles control these changes in the scrotal surface area. Namely, the dartos muscle, which contracts to wrinkle the scrotal skin, coupled with the cremaster muscle, which contracts to elevate the testes.
Structure
A scrotum is a highly pigmented, muscular sac that encloses the testes. A ridgelike seam called the raphe divides it into two compartments. Each compartment of the scrotum contains one testis, one epididymis, and the testicular end of a spermatic cord.
Internal organs of the male reproductive system
1. Testes
Location
In utero, the testes develop in the abdominal cavity of the fetus. After that, they cross the inguinal canal and enter the scrotal sac. This happens in the 8th month of fetal life and is called the descent of the testes. But what happens if the child is prematurely born or this descent does not occur? Let‘s read about it.
What are undescended testes?
Cryptorchidism (or undescended testes) is a common childhood condition where the child is born without both the testes in the scrotal sac. In the majority of cases, no action is required as the testes will migrate down into the scrotum during the first 3–6 months. There are, however, a small number of cases where the testes remain undescended unless treated. In fact, research suggests that children with undescended testes may have problems associated with fertility. In addition, there is an increased risk of testicular cancer in such children.
Structure
The testes are the site of sperm production in the male reproductive system. Not to mention, they are homologous to the ovaries in females. They are oval in shape, and each testis is about 4.5 cm long, 2.5 cm wide, and 3 cm thick. Both the testes hang on either side of the penis. Besides, it is usual for one to hang lower than the other.
In each testis, there are about 200–300 lobules. Within each lobule, there are 1–4 convoluted loops of germinal epithelial cells called the seminiferous tubules. In fact, these tiny tubules are the site of sperm production. Between the tubules, there are groups of interstitial cells (or Leydig cells) that secrete the hormone testosterone.
At the upper pole of the testis, the tubules merge to form a single, straight tubule. As shown in the figure, the Rete testis connects these straight tubules to the efferent ducts. Sperm then pass through the efferent ducts and enters the first portion of the duct system, the epididymis. Finally, sperm leaves the testes through the ductus deferens (vas deferens) in the spermatic cord.
The spermatic cord suspends the testes in the scrotum. Each cord contains a testicular artery, testicular veins, lymphatics, a deferent duct, and testicular nerves. In addition, the cord extends through the inguinal canal.
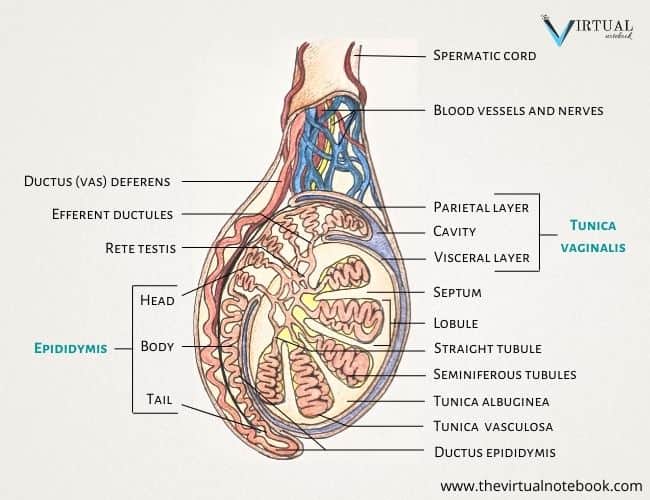
Layers
Testes are surrounded by three layers of tissue:
- Tunica vaginalis. This is a double membrane (a parietal and a thin visceral layer) forming the outer covering of the testes. It is a down growth of the abdominal and pelvic peritoneum.
- Tunica albuginea. This is a fibrous covering beneath the tunica vaginalis that covers the testes. It also invaginates to form septa that divide the testis into 300 to 400 structures called lobules.
- Tunica vasculosa. This is the inner layer of the testes which surrounds the lobules. It consists of a network of capillaries that are supported by the delicate connective tissue.
Function of testes
The testes perform two very important functions. They:
- Produce sperm cells, and
- Secrete androgen hormones, most importantly testosterone.
2. Duct system
After leaving the testes, the sperm travels through a system of ducts. The epididymis, ductus deferens, ejaculatory duct and lastly, the urethra. This duct system transports sperm and is also involved in ejaculation, the process by which semen is expelled from the penis.
a) Epididymis
The epididymis is a comma‐shaped duct (~4 cm long). In addition, it lies in the posterior lateral aspect of the testes. To point out, it is the site of sperm maturation and storage. It takes ~14 days for sperms to complete their maturation and become motile. If ejaculation does not occur, sperm cells remain there for several months and are eventually reabsorbed.
As shown in the figure, the epididymis includes the head, body, and tail regions. The head of the epididymis contains the efferent ductules of the testis, which are highly coiled. The body and tail are made up of a single duct, ductus epididymis, which is highly coiled as well. At the lower end of the tail, this duct becomes continuous with the vas deferens.
b) Vas deferens (or ductus deferens)
The vas deferens is a long (~45 cm long) muscular tube that extends from the tail of the epididymis. There are two vas deferens that connect the left and right epididymis. In addition, it is wider (2.5mm) and less convoluted than the epididymis.
The vas deferens enters the pelvic cavity through the inguinal canal. After which, it passes along the lateral side of the bladder, over the ureter, and then along with the posterior bladder. As shown in figure 1, it ends in a sac-like wider area called the ampulla, which helps nourish the sperm. The vas deferens then joins the seminal vesicle to become the ejaculatory duct. This duct then passes into the prostate gland, discharging its fluid into the urethra.
c) Ejaculatory duct
There are two ejaculatory ducts that are ~2 cm long. To point out, the union of the vas deferens and seminal vesicle give rise to two such ducts. Both ducts pass through the prostate gland and then join the single urethra. As a matter of fact, the same layers of tissue make the walls of the ejaculatory ducts as the seminal vesicles do.
d) Urethra
The last part of the duct system that makes up the male reproductive system is the urethra. The urethra connects the urinary bladder to the external body surface.
The male urethra provides a common pathway for the flow of urine and semen. Whereas the female urethra has the sole purpose of carrying urine from the bladder to the outside of the body. In addition, the length of the urethra is much shorter in females than that in males. The male urethra is about 19–20 cm long and consists of three parts.
- The prostatic urethra originates at the internal urethral orifice present at the end of the bladder. Also, it surrounds the prostate gland.
- The membranous urethra is the shortest and narrowest part. It extends from the prostate gland to the bulb of the penis.
- The spongy or penile urethra lies within the corpus spongiosum of the penis. At last, it ends with the external urethral orifice present in the glans penis.
Key point: The mucosa of the urethra contains several small mucus-secreting glands called the urethral glands. They empty into the urethra and contribute to semen as well.
Male accessory glands
There are 3 main accessory glands in the male reproductive system. Namely, seminal vesicles, the prostate gland, and bulbourethral glands. The bulk of the semen is produced by the following accessory glands, and sperm make only 5% of the final volume of semen.
1. Seminal vesicles
The seminal vesicles are two small (5 cm long) fibromuscular pouches. The paired structures are found on the posterior side of the urinary bladder near the ampulla. Each seminal vesicle converges with the ductus deferens to form a short ejaculatory duct.
Key point: Each seminal vesicle is ~15 cm long but is tightly coiled and folded until it becomes 5 cm long.
Function of seminal vesicles
The seminal vesicles contract and expel their stored contents during ejaculation. Seminal fluid— a thick, yellowish secretion that makes up ~60–70% of total semen volume, contains:
- Fructose, which provides energy to the sperm to enhance motility.
- Prostaglandins, which stimulate smooth muscle contractions in both the male and female reproductive tracts. Besides, it increases sperm viability.
- It also contains coagulating proteins and enzymes, which help in forming a temporary clot of semen in the female reproductive tract.
Key point: the pH of the seminal fluid is alkaline (~7.2–7.5) in nature to protect the sperm in the acidic environment of the vagina.
(adsbygoogle = window.adsbygoogle || []).push({});2. Prostate gland
The prostate gland in the male reproductive system is homologous to the female paraurethral glands (or skene glands). It lies in front of the rectum and at the base of the urinary bladder, surrounding the prostatic urethra.
Structure
The gland is approximately the size of a walnut (~4 cm). It weighs about 8 g in youth but progressively enlarges with age. By the age of 50, it is likely to weigh about 40 g.
Roughly two-thirds of the prostate is glandular in structure, and the remaining third is fibromuscular (i.e., fibres plus muscle). During ejaculation, the glandular tissue of the prostate secretes an alkaline fluid that helps maintain sperm motility. On the other hand, prostatic smooth muscle contracts and push the stored fluid out into the urethra.
The gland is surrounded by a true internal connective tissue capsule and a false external capsule. The true capsule is continuous with the stroma of the gland and the false capsule is a continuation of the pelvic fascia. Note that it is called a false capsule as it rather resembles the thin connective tissue known as adventitia in the large blood vessels and is not a real capsule.
To sum up, the prostate consists of 20–30 tubular glands enclosed in a mass of smooth muscle fibres and dense elastic connective tissue. This is why it feels really elastic to the touch in the rectal exam.
What is benign prostatic hyperplasia (BPH)?
Benign prostatic hyperplasia (BPH) is an increase in the size of the prostate without the presence of malignancy. It is much more common with advanced age but may happen with earlier age (>40 years). Approximately 40% of men in their 60s have some degree of BPH. Moreover, by the age of 80, the number of affected individuals jump to as many as 80%.
Although the prostate normally doubles in size during puberty, this enlargement does not usually cause problems. However, abnormal growth of the prostate or BPH can cause constriction of the urethra. This constriction further leads to a number of lower urinary tract symptoms. For example, a frequent and intense urge to urinate, a weak stream, and a sensation that the bladder has not emptied completely.
Treatments for BPH attempt to relieve the pressure on the urethra so that urine can flow more easily. Although mild to moderate symptoms are treated with medication, surgery is performed in case of severe enlargement of the prostate.
Prostate cancer
Sometimes an enlarged prostate is secondary to prostate cancer. Also, it is the second most common cancer in men. Although there is no link between BPH and prostate cancer, the symptoms are similar. However, some forms of prostate cancer grow very slowly and thus may not require treatment. Aggressive forms of prostate cancer, in contrast, involve metastasis to organs like the lungs and the brain.
Screening for prostate cancer usually includes a blood test and a digital rectal exam in which a medical professional palpates the prostate and checks for unusual masses. If a mass is detected, the cancer diagnosis is confirmed by biopsy of the cells.
Function of the prostate gland
The prostate gland secretes a thin, milky fluid that makes up about 30% of the volume of semen. It contains:
- Citrate, a sugar that the sperm use as a nutrient to make ATP.
- Prostate-specific antigen (PSA) and other enzymes. At first, the enzymes thicken the semen in the vagina to retain it close to the female reproductive tract. The temporary clotting provides time for the sperm to utilize fructose secreted by the seminal vesicles. This, in turn, increases sperm motility. Later, PSA dissolves the clot of semen, which helps the sperm to move deeper into the tract.
- Antimicrobial chemicals. They inhibit the growth of bacteria in the female reproductive system. This, in turn, decreases the risk of infection.
3. Bulbourethral glands
The paired bulbourethral glands are also known as the Cowper’s glands. They are about the size of a pea (~1 cm). In addition, they are located below the prostate gland on both sides of the membranous urethra. Furthermore, each round gland has a short duct that connects to the penile urethra. To point out, bulbourethral glands grow smaller with age, unlike the prostate gland and are very small in older men.
Function of bulbourethral glands
In response to sexual stimulation, they secrete an alkaline, mucus-like fluid. This fluid:
- Helps to clean urine residues from the penile urethra,
- Provides lubrication to both male and female sex organs, and
- Neutralizes the acidity of the vagina.
This fluid is released shortly before the release of semen. It is, therefore, sometimes called pre–ejaculate. It is important to note that in addition to the lubricating proteins, bulbourethral fluid can pick up sperm already present in the urethra. Therefore, it may be able to cause pregnancy.
Key point: You have probably noticed that the secretions of the male reproductive glands are alkaline. This is important because the female vagina has an acidic pH due to the natural bacterial flora. The alkalinity of seminal fluid helps neutralize the acidic vaginal pH and permits sperm motility. This might otherwise be an unfavourable environment.
Site of sperm storage and maturation
Sperms are produced in the seminiferous tubules of the testes. These tubules connect to the duct system passing through the epididymis, which is the site of sperm storage and maturation. It takes ~14 days for sperm to become mature and motile. Sperm then travels through the ductus deferens and can be stored in there for several months in case ejaculation does not occur. The remaining sperms that are not released are ultimately reabsorbed.
What is the pathway of sperm?
In the male reproductive system, sperms travel through different structures of the testes until ejaculation occurs, which takes place in two phases:
- In the 1st stage, sperms are expelled from the epididymis and pushed to the beginning of the urethra.
- At first, the muscles around the epididymis and ductus deferens contract. This helps to push the sperm into the prostate. The entire process is accomplished by strong nerve impulses received from the penis. Once the process begins, the ejaculation becomes unstoppable.
- It should be noted that the seminal fluid is not released from the various accessory glands at the same time. Initially, a small amount of mucus-like secretion is passed from the bulbourethral and urethral glands. These secretions flush out the urethra and prepare it for the passage of sperm.
- Next follows the contractions of the prostate gland. After that, a muscle in the walls of the seminal vesicles also contract. This results in the addition of their contents to the fluid passing through the ejaculatory duct.
- In the 2nd stage, the semen is moved through the urethra and expelled from the body.
- Then begins the spasmodic contraction in the spongy part of the urethra. After that, the semen is expelled through the external urethral sphincter.
- After the bulk of the sperm cells have passed, more fluids follow and again flush out the urethra. In this phase, muscles at the base of the penis contract every 0.8 seconds. This forces the semen out of the penis in up to 5 spurts.
The secretions of the testes and accessory glands are produced under the influence of the male hormone testosterone. Without sufficient testosterone levels, the glands degenerate and cannot secrete fluids.
Sperm count
The total volume of the ejaculate averages between 2-5 ml. It may contain 40-100 million sperm/ml. The Sperm comprise only 5-10% of the final ejaculate. The remainder constitutes mainly seminal (50–60%) and prostatic fluids (20–30%). The other components of semen include nutrients, water, salts, waste products of metabolism, and cellular debris.
Sources
Amerman, Erin C. “The reproductive system.” (2016). Human anatomy and physiology. global edition. 1053–1064.
Ian Pete and Muralitharan Nair. (2016). “The reproductive systems.” Fundamentals of anatomy and physiology: for nursing and healthcare students. 2nd edition. 373–382.
Openstax college. (2013). “The reproductive systems.” Anatomy and physiology. 1219–1226.
Ross and Wilson. (2014). “The reproductive systems.” Anatomy & physiology in health and illness. 12th edition. 459–463.
Sanders, Valerie C. Scanlon and Tina. (2007). “The reproductive system.” Essentials of anatomy and physiology. 5th edition. 456–462.
InformedHealth.org [Internet]. Cologne, Germany: Institute for Quality and Efficiency in Health Care (IQWiG); 2006-. “How does the prostate work?” 2011 Feb 15 [Updated 2016 Aug 23]. Available from: www.ncbi.nlm.nih.gov/books/NBK279291/