The Immune System of humans consists of a variety of cells and tissues. The cells of the immune system work together as a defence against infection and diseases. The immune system cells develop from stem cells (HSCs) in the bone marrow and become different types of white blood cells. These cells are normally present as circulating cells (in blood and lymph) and as scattered cells (in all tissues).
Cells of the Immune System
All the cells of the immune system arise from a single hematopoietic stem cell (HSC). Actually, HSC can give rise to three different types of progenitor cells, namely, lymphoid progenitor, myeloid progenitor and erythroid progenitor. Basically, lymphoid and myeloid progenitors give rise to immune cells and erythroid progenitor gives rise to other types of blood cells.
In this article, we will discuss lymphoid and myeloid progenitors in detail.
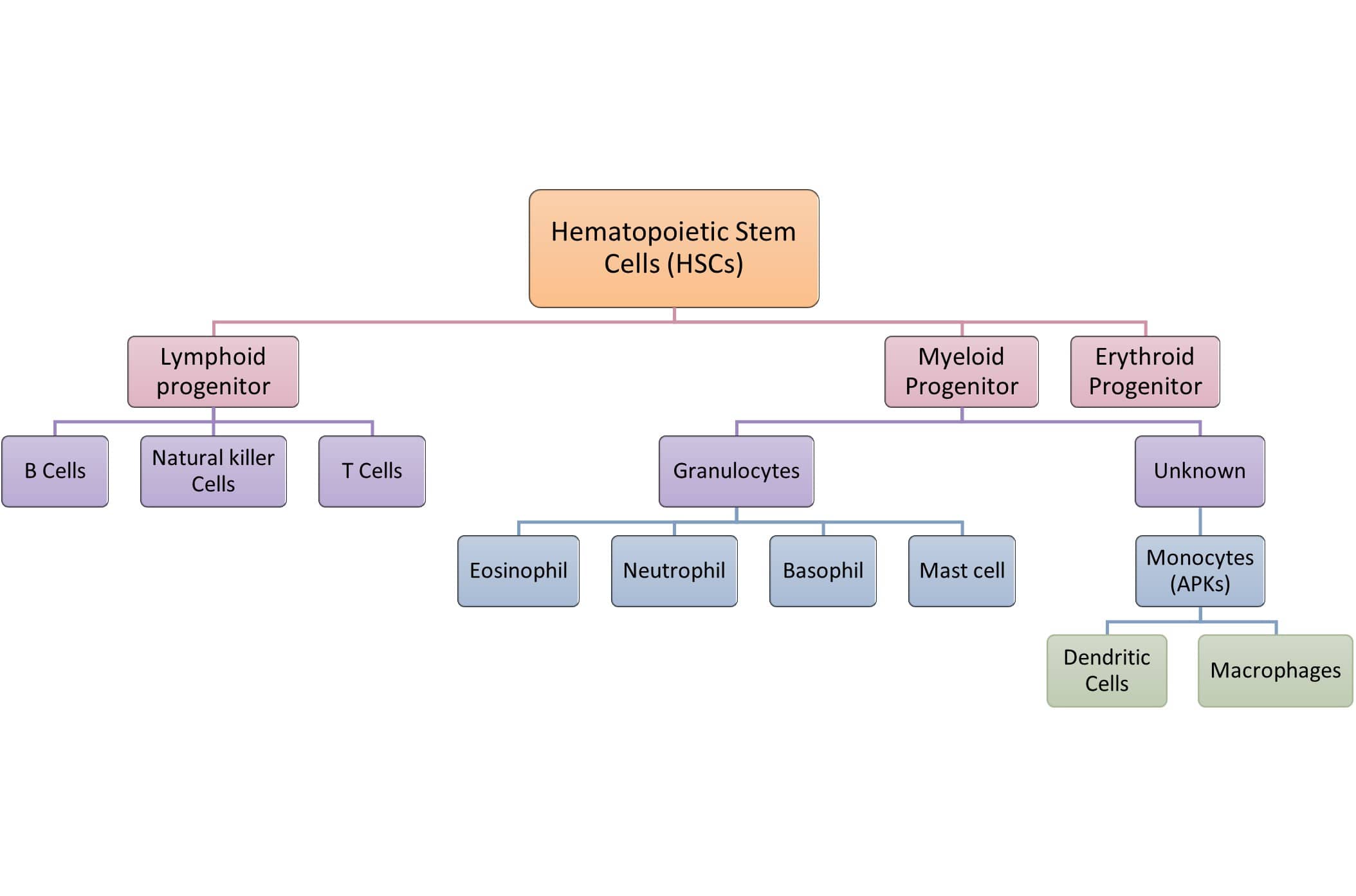
- LYMPHOID PROGENITORS: they give rise to three types of immune cells.
- B cells
- Natural killer cells
- T cells
- MYELOID PROGENITORS: they give rise to two types of immune cells that have further sub-classes.
- Granulocytes
- Eosinophils
- basophils
- Neutrophils
- Mast cells
- Unknown cells
- Antigen-presenting cells (Monocytes)
- dendritic cells
- macrophages
- Antigen-presenting cells (Monocytes)
- Granulocytes
- ERTHROID PROGENITORS
- Megakaryocytes
- platelets
- Erythroblasts
- erythrocytes (RBCs)
- Megakaryocytes
Myeloid cells and NK cells are members of the innate immune system and are the first cells to respond to infections. Lymphocytes are members of the adaptive immune response and generate a refined antigen-specific immune response which also produces immune memory. Macrophages and dendritic cells are monocytes that have non-granular cytoplasm. Monocytes circulate in the blood for about one to three days, and then usually enter the body’s tissues, where they differentiate into macrophages and dendritic cells.
LYMPHOID PROGENITORS
Lymphoid progenitors give rise to B cells, T cells and natural killer cells. B cells and T cells fall under lymphocytes.
Cells of Adaptive Immune System: Lymphocytes
Lymphocytes are ovoid cells, about 8-12 µm in diameter, and are mobile and circulate throughout the body. The lymphocytes occupy a very special place among the white blood cells that participate in one way or another in immune reactions due to their ability to interact specifically with antigenic substances and to react to nonself antigenic determinants. In addition, they also contribute to the memory of the immune system. Therefore, lymphocytes are the mediators of humoral and cellular immunity. There are various sub-types of lymphocytes that differ in terms of origin, lifespan, preferred areas of settlement within the lymphoid organs, surface structure, and function.
They represent 20% to 40% of circulating white blood cells and 99% of cells in the lymph. Lymphocytes differentiate from stem cells in the fetal liver, bone marrow, and thymus into two main functional classes:
- T cells
- B cells
Depending upon where they undergo their development and proliferation, they are grouped into the above two classes. For example, B cells develop in the bone marrow and T cells develop in the thymus. Hence, they have named B cells (B derived from bone marrow) and T cells (T- thymus). Both B and T lymphocytes are structurally alike but functionally different. They are present in the peripheral blood and in all lymphoid tissues.
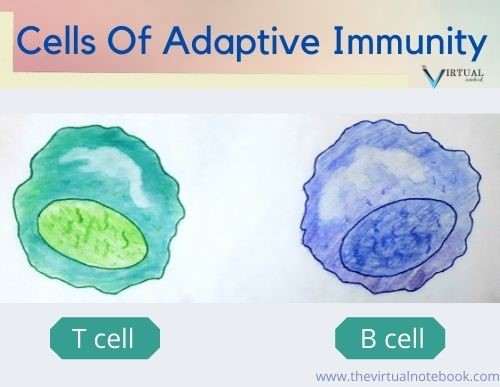
1. T lymphocytes/ T cells
T cells are the cells of adaptive immunity.
Role: they participate directly in the immune responses as well as in arranging and regulating activities of other cells.
Characteristics
- T-cells develop in the bone marrow but complete their development in the thymus.
- they represents 65–80% of the circulating pool of small lymphocytes.
- they can live longer than B cells. Longlasting lymphocytes are particularly important because of their involvement on immunological memory.
- T cells are present in the inner subcortical regions but not in the germinal centers of the lymph nodes.
- they are different from other lymphocytes as they have a T cell receptor (TCR) on their surface. TCR do not recognize whole antigens, but instead react only to small fragments of antigens.
- they can target and selectively destroy virus-infected cells and cancer cells.
- T cells do not produce any antibody.
Sub-classes
There are two main and two rare sub-classes of T cells:
- MAIN
- Helper T cells (CD4+)
- Cytotoxic T cells (CD8+)
- RARE
- TREG cells
- γδ T-cells
1.1 Helper T cells (CD4+)
They are also known as CD4+ cells. Helper T (Th) cells are mainly present in the thymic medulla, tonsils, and blood. Basically, they constitute about 65% of peripheral T cells. These cells have no cytotoxic activity and do not kill infected cells or clear pathogens directly. They instead control the immune response by directing other cells to perform these tasks.
CD4+ cells recognize a nonpeptide-binding portion of MHC class II molecules. Hence, CD4+ T cells are restricted to the recognition of pMHC class II complexes.
Function
- These cells help B cells and other T cells to multiply into large clones and carry out their role in immune response.
- Th-1 cytokines activate cytotoxic inflammatory and delayed hypersensitivity reactions.
- Th-2 cells help in the production of interleukins which encourage production of antibodies especially IgE.
- Th-2 cytokines are associated with regulation of strong antibody and allergic responses.
1.2 Cytotoxic T cells (CD8+)
They are also called cytotoxic T (Tc) and suppressor T (Ts) cells. They account for approximately one-third of all mature CD3+ cells. These are present mainly in the human bone marrow and gut lymphoid tissue. CD8+ T glycoprotein of T cells recognizes a nonpeptide-binding portion of MHC class I molecules. Hence, CD8+ T cells are restricted to the recognition of pMHC class I complexes.
Point to remember: Both CD4+ and CD8+ T cells recognize a nonpeptide-binding portion of MHC molecules. But CD4+ recognize a portion of MHC class II molecules whereas CD8+ recognize the MHC class I molecule portion.
Function
They perform mainly cytotoxic functions.
- CD8+ T cells kill virus infected cells.
- They also kill tumor cells and allograft cells.
1.3 Regulatory T-cells (TREG cells) or supressor T cells (former name)
They provide tolerance to self-antigens (peripheral tolerance), and prevent the development of autoimmune disease.
Surface markers: TREG cells possess surface markers such as CD4, CD25 and Foxp3. Deficiency of Foxp3 receptors leads to a severe form of an autoimmune disease known as Immune dysregulation, Polyendocrinopathy, Enteropathy X-linked (IPEX) syndrome.
1.4 γδ T-cells
They constitute 5% of total T-cells, express γ/δ chains of TCR chains; instead of α/β chains.
- They lack both CD4 and CD8 molecules. Also, they do not require antigen processing and MHC presentation of peptides.
- They are part of innate immunity as the γδ receptors exhibit limited diversity for the antigen.
- γδ T cells are usually found in the gut mucosa, as intraepithelial lymphocytes (IELs).
- The function of γδ T-cells is not known, they may encounter the lipid antigens that enter through the intestinal mucosa.
See also:
B lymphocytes (B cells)
B cells acquired their name from their site of maturation, bursa of fabricus in birds and bone marrow in mammals. Unlike T cells, they can be morphologically distinguished by their synthesis and display of the B-cell receptor (BCR), a membrane-bound immunoglobulin (antibody) molecule that binds to the antigen.
Each B cell shows a surface antibody with a unique specificity, and each of the approximately 1.5–3 x105 molecules of surface antibody has identical binding sites for antigen. B lymphocytes also can improve their ability to bind antigen through a process known as somatic hypermutation and can generate antibodies of several different functional classes through a process known as class switching.
Ultimately, activated B cells differentiate into effector cells known as plasma cells. They can produce and secrete large amounts of immunoglobulin but do not express membrane immunoglobulins.
A single cell is capable of secreting from a few hundred to more than a thousand molecules of antibody per second. Plasma cells do not divide and, although some long-lived populations of plasma cells are found in bone marrow, many die within 1 or 2 weeks.
B cells are the only cell of the immune system that are specialized to secrete antibodies and, therefore, constitute the principal mediators of the humoral (i.e., antibody) immune response.
Function
- Activated B cells (plasma cells) produces large amount of immunoglobulins specific for the epitope of the antigen.
- Plasma cells also produces memory cells which remain alive (in resting stage) for months and some even for years.
Cells of Innate Immune System: Myeloid cells and natural killer cells
Myeloid progenitors give rise to two types of cells: granulocytes and unknown cells.
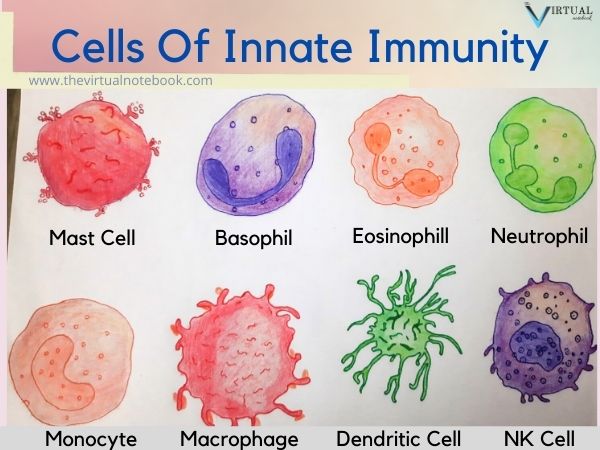
1. Granulocytes
Granulocytes are a type of white blood cell that has granular proteins. They comprise 3-8% of WBCs in the blood. Further, they give rise to four types of granular cells: basophil, eosinophil and neutrophil and mast cell.
1.1 Neutrophils
Neutrophils are the largest subpopulation of white blood cells (leukocytes). They differentiate in the bone marrow. After that, neutrophils will move into the peripheral blood and circulate for 7 to 10 hours before migrating into the tissues, where they have a life span of only a few days.
They are the first cells that act at the site of tissue damage to eliminate pathogens especially bacteria by phagocytosis. Once in tissues, neutrophils phagocytose (engulf) bacteria very effectively, and also secrete a range of proteins that have antimicrobial effects and tissue remodelling potential.
1.2 Eosinophils
Eosinophils constitutes 1-3% of circulating white blood cells (leukocytes). They are motile phagocytic cells that can migrate from the blood into the tissue spaces. Their phagocytic role is significantly less important than that of neutrophils. These cells are present in high concentrations in allergic reactions and during parasitic infections, including worms.
1.3 Basophils
Basophils are the least common type of granulocyte. Unlike neutrophils and eosinophils, they are nonphagocytic cells that contain large granules filled with basophilic proteins. Basophils constitute less than 1% of white blood cells. They release the contents of their granules in response to the binding of circulating antibodies. Histamine, one of the best-known proteins in basophilic granules, increases blood vessel permeability and smooth muscle activity. Basophils play key pathogenic roles in allergic reactions.
1.4 Mast cells
Like basophils, they constitute less than 1% of white blood cells. Mast cells mature only after they leave the blood.
Mast cells are present in a wide variety of tissues, including the skin, connective tissues of various organs, and mucosal epithelial tissue of the respiratory, genitourinary, and digestive tracts. Like circulating basophils, these cells have large numbers of cytoplasmic granules that contain histamine and other pharmacologically active substances. Mast cells also play an important role in the development of allergies.
2. Antigen Presenting Cells (APKs)
Antigen-presenting cells (APCs) include :
- Macrophages and
- Dendritic cells.
2.1 Macrophages (accessory cells)
Macrophages are phagocytic cells. These are not antigen-specific and hence also called accessory cells of the immune system. Monocytes and macrophages are believed to be closely related. The monocyte is considered a leukocyte in transit through the blood, which when fixed in the tissue will become a macrophage. They are closely related but there are fine differences too. These are as follows:
- Macrophages are larger than monocytes. They are atleast 5-10 fold bigger than monocytes.
- They are different in terms of cellular content too. Macrophages contain more lysozymes, organelles, enzymes and cytokines.
- Macrophages produces higher levels of hydrolytic enzymes.
- Lastly, they have greater phagocytic activity and have a longer life in tissues (months to years).
Functions
Macrophages perform three main functions:
- Phagocytosis
- Antigen presentation
- Cytokine production
2.2 Dendritic cells
Dendritic cells are so named because of their resemblance to neuronal dendrites. Like neuronal dendrites, they have many long, narrow processes which make them very efficient at making contacts with foreign materials. Basically, they are bone marrow-derived cells that express class II MHC proteins and present antigen to CD4+ T cells.
They act as a messenger between the innate and adaptive immune systems. Dendritic cells are present in those tissues that are in contact with the external environment. For example, the skin and the inner lining of the nose, intestine and stomach. Upon activation, they migrate to the lymph node. After that, they interact with B cells and T cells to initiate the adaptive immune response.
Function
- The main function of the dendritic cell is to process the antigen material and present it on the cell surface to the T cells.
Natural killer cells (NK)
Natural killer (NK) cells are large granular lymphocytes that constitute 10–15% of total lymphocytes. They are efficient cell killers and attack some tumor cells and virally infected cells.
Characteristics
- They are large granular lymphocytes.
- NK cells develop within the bone marrow and lack T-cell receptor, but possess another set of receptors called killer activation receptors and killer inhibition receptors.
- Prior exposure does not increase the activity.
- Thymus is not required for development.
- Number remains normal in severe combined immunodeficiency disease.
Function
- The main function of NK cells is to kill tumor cells.
- They also kill viras-infected cells.
References
Bhatia, Rajesh, and Rattan Lal Ichhpujani. “Cells of the Immune System.” Essentials of Medical Microbiology. 4th ed. Jaypee Brothers, 2008. 95-99.
Owen, Judith A., Jenni Punt, and Sharon A. Stranford. “Cells, Organs and Microenvironments of the Immune System.” Kuby Immunology. 7th ed. W.H. Freeman, 2013. 27-54.
Parija, Subhash Chandra. “Structure and Function of the Immune System.” Textbook of Microbiology & Immunology. 2nd ed. Elsevier, 2012. 122-33.
Virella, Gabriel. “Cells and Tissues Involved in the Immune Response.” Medical Immunology. 5th ed. Marcel Dekker, 2001. 11-30.
How to order this book