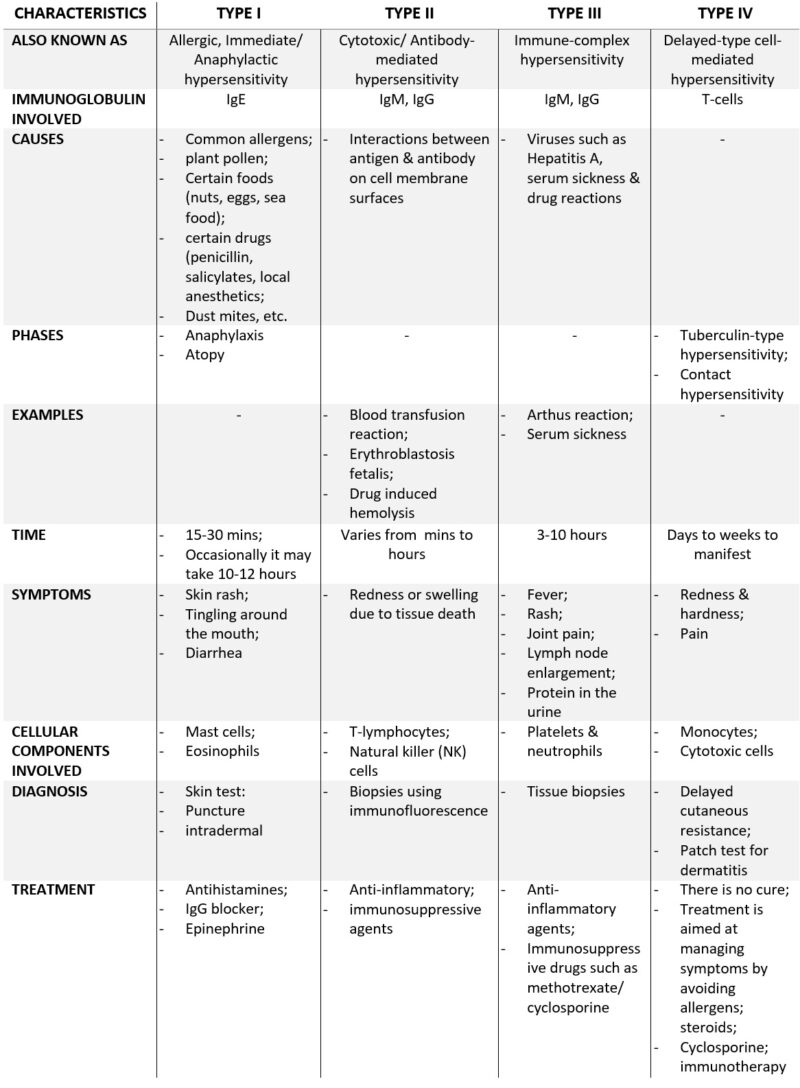
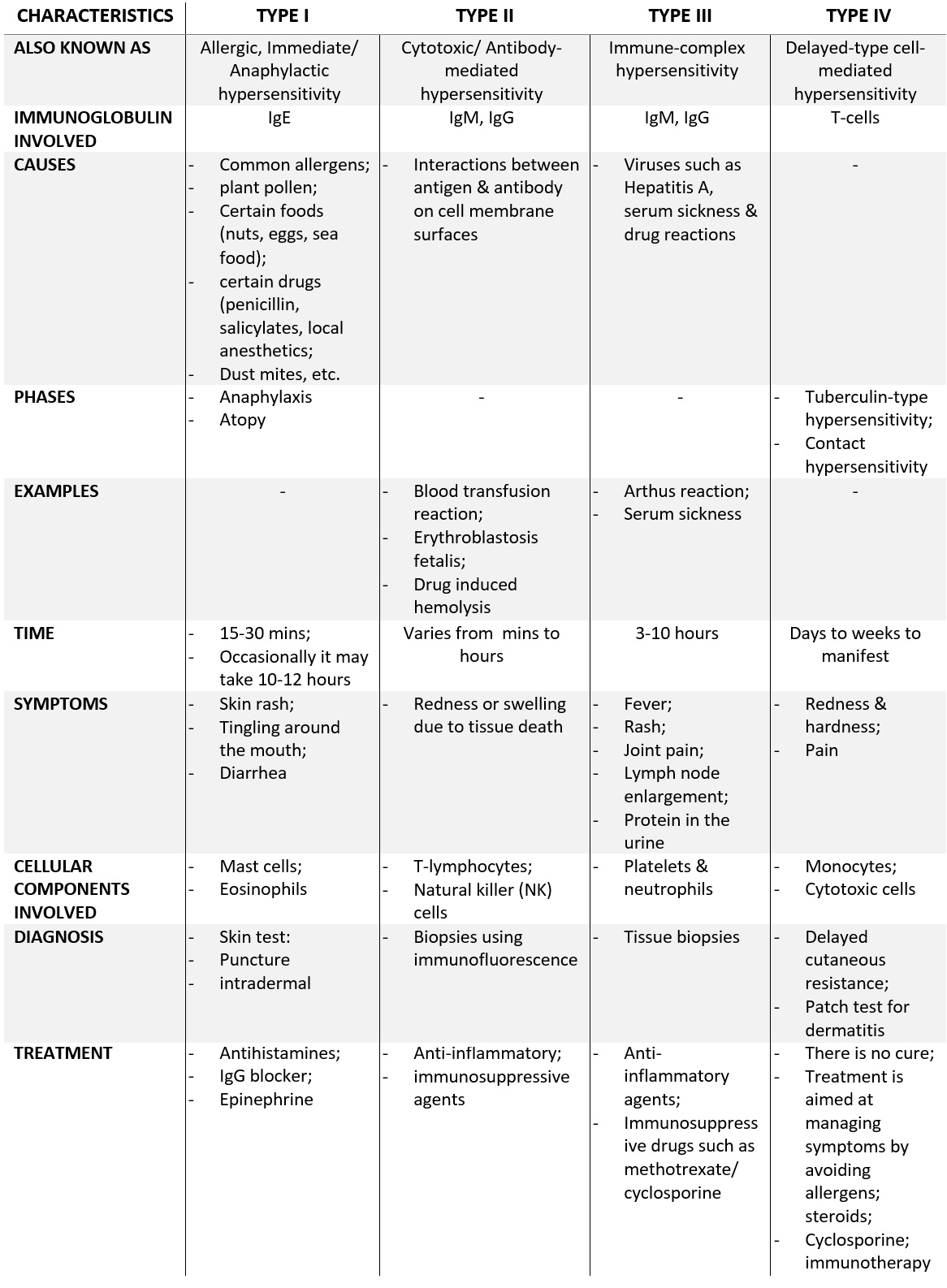
Hypersensitivity refers to extreme physical sensitivity to particular substances or conditions. It is the undesirable reactions produce by the normal immune system in the form of allergies and autoimmunity. In other words, it is an over-reaction of the immune system and these reactions may be damaging, uncomfortable, or occasionally fatal. You can divide hypersensitivity into five types on the basis of their mechanism and of course, the time taken for the reaction.
- type I hypersensitivity,
- type II hypersensitivity,
- then, type III hypersensitivity,
- type IV hypersensitivity
- and lastly, type V hypersensitivity.
Types I, II, and III are antibody-mediated (immediate) hypersensitivity, while type IV is cell-mediated (delayed) hypersensitivity reactions.
TYPE I HYPERSENSITIVITY
Type I hypersensitivity reaction is commonly called an allergic or immediate hypersensitivity reaction. This reaction is always rapid and can occur within minutes of exposure to an antigen. Type I hypersensitivity reactions are initiated by the interactions between an IgE antibody and a multivalent antigen.
(IgE antibodies are class of antibodies that produces in allergic reactions and multivalent antigen is an antigen molecule with more than one identical epitope per molecule)
Type I hypersensitive reactions can induce by a special type of antigen refer to as allergens which have all the hallmarks of the
Common allergens for type I hypersensitivity are plant pollen, foods (nuts, eggs, seafood, etc.), certain drugs (penicillin, Salicylates, local anaesthetics, dust mites, etc.
Type I reaction can occur in two forms:
- anaphylaxis, and
- atopy.
The precise component of why some people are more prone to Type 1 hypersensitivity is unclear. However, it has been shown that such individuals preferentially produce more lymphocytes or TH2 cells which in turn favor the change of class
1. Anaphylaxis
It is an acute and potentially fatal immediate hypersensitivity reaction. The time of onset of symptoms depends on the level of hypersensitivity and the site of exposure to the antigen. Generally, it affects skin, respiratory tract and cardiovascular system. Plasma cell secretes IgE in response to allergen-specific TH4 cells. This class of antibody binds with high affinity to Fc receptor on the surface of tissue mast cells and basophils. Binding of IgE to the mast cells is also known as sensitization. IgE-coated mast cells can activate on repeat antigen encounter. The primary cellular component in this hypersensitivity are the mast cell, eosinophils, and basophil.
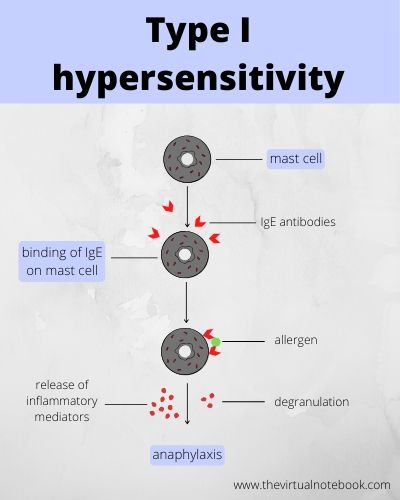
Further. anaphylaxis has two phases:
- immediate
- late
Immediate phase
This phase is characterized by degranulation and release of pharmacologically active mediators within minutes of re-exposure to the same antigen. Histamine is the principal biogenic amine that causes rapid vascular and smooth muscle reactions.
Late phase
This phase begins to develop 4–6 hours after the immediate phase reaction and can persist for 1–2 days. It is identified by the infiltration of neutrophils, macrophages, eosinophils, and lymphocytes to the site of reaction.
2. Atopy
Unlike anaphylaxis, atopy is periodic and nonfatal immediate hypersensitivity reaction. Atopic individuals produce high levels of IgE in response to allergens as compared to normal individuals who do not. An example of atopic reactions is bronchial asthma. Atopic hypersensitivity does not transfer through lymphoid cells but it can transfer by serum.
Symptoms
Some of the common symptoms are skin rashes, tingling around the mouth, diarrhoea, etc., It can affect various organs of the body including skin (Urticaria and Eczema), eyes (conjunctivitis) and nose (rhinorrhea.
Time
Generally, it took 10-30 minutes for the symptoms to appear and occasionally it may take up to 10-12 hours.
Diagnosis
Its diagnosis may include skin tests like puncture and intradermal. In addition, measurement of total IgE and IgE antibodies, specific against suspected allergens, also performed.
Treatment
Antihistamines are used for the treatment of type I hypersensitivity. These medications block histamine receptors on cell membrane surfaces.
Treatment for anaphylactic symptoms is injection with epinephrine, a potent neurotransmitter and hormone that effectively halts the immune response.
IgG blockers are also used to treat type I hypersensitivity.
TYPE II HYPERSENSITIVITY
Type II hypersensitivity is also known as cytotoxic hypersensitivity or antibody-mediated hypersensitivity reactions. Also, it may affect a variety of organs and tissues. Type II hypersensitivity reactions involve antibody-mediated destruction of cells by immunoglobulins of heavy chain classes other than IgE.
Further, see: Immunoglobulin classes and structure
Antibody bound to a cell-surface antigen can induce death of the antibody-bound cell by three distinct mechanisms.
- First, the antibody bound to a cell surface can activate the complement system, creating pores in the membrane of a foreign cell.
- Secondly, antibodies can mediate cell destruction by the antibody-dependent cell-mediated cytotoxicity (ADCC). In this process, cytotoxic cells with Fc receptors bind to the Fc region of antibodies on target cells and promote killing of the cells.
- Finally, the
antibody bound to a foreign cell alsoserve as an opsonin, enabling phagocytic cells with Fc or C3b receptors to bind and phagocytose the antibody-coated cell
Examples
- Blood transfusion/transfusion reactions: When transfusion with mismatch blood occurs, a transfusion reaction takes place due to the destruction of the donor RBCs through the iso-hemagglutinins against the foreign antigen.
- Erythroblastosis Fetalis: it develops when maternal antibodies specific for fetal blood group antigens cross the placenta and destroy fetal RBCs. As a result, severe hemolysis occurs, leading to anaemia and hyperbilirubinemia, which can even be fatal.
- Drug-Induced Hemolysis: Certain drugs (such as penicillin, quinidine, phenacetin, etc.) may induce hemolysis of red blood cells. They attach to the surface of red blood cells and induce the formation of IgG antibodies. These autoantibodies then react with red blood cell surface, causing hemolysis.
Symptoms
Redness and swelling are major symptoms under this categories. Generally, it develops from any where between minutes to hours.
Treatment
The treatment includes anti-inflammatory and immunosuppressive agents.
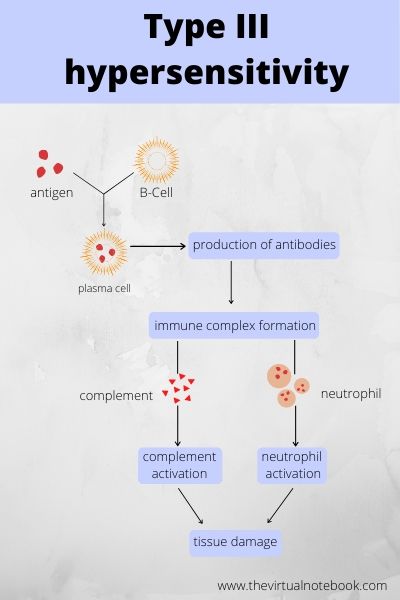
TYPE III HYPERSENSITIVITY (immune-complex)
Type III reactions are results of antigen-antibody immune complexes, which induce an inflammatory reaction in tissues. The Reaction between the various antigens and antibodies in the body gives rise to the formation of immune complexes. In the normal condition, the mononuclear-phagocyte system removes these immune complexes through the participation of RBC.
In certain cases, these immune complexes are beyond the reach of phagocytic clearance capacity. As a result, they can increase and cause disease.
Immune complex deposition happens at:
- on blood vessel walls
- in the synovial membrane of joints
- on the glomerular basement membrane of the kidneys
- on the choroid plexus of the brain
- sometimes, immune complexes form at the site of inflammation itself
Immune complexes fix and activate the complement system. Complement fixation results in the production of the anaphylatoxin chemokines C3a and C5a that stimulate the
Examples
- Arthus reaction
- Serum sickness
Symptoms
As a result of type III hypersensitivity, complex deposition in the tissues can give rise to symptoms such as fever, rashes, joint pain, lymph node enlargement, and protein in the urine.
Time
Generally, it requires 3-10 hours for the symptoms to occur.
Treatment
The treatment includes anti-inflammatory agents. In addition, Immunosuppressive drugs such as methotrexate and cyclosporin are also used in some cases.
TYPE IV HYPERSENSITIVITY
you can also call it delayed-type cell-mediated hypersensitivity reactions. It starts hours or days after primary contact with the antigen and often lasts for days. There is a large influx in non-specific inflammatory cells, in particular, macrophages in this reaction. It differs from the other types of hypersensitivity because it mediates through cell-mediated immunity. This reaction occurs due to the activation of specifically sensitized T lymphocytes rather than antibodies.
In 1890, Robert Koch observed this type of hypersensitivity in tuberculosis as a localized reaction. It is also known as the tuberculin reaction. Later, on the realization that the reaction can be induced in various pathologic conditions, it was renamed as delayed–type hypersensitivity.
DTH (Delayed-Type Hypersensitivity) response begins with an initial sensitization by antigen, followed by a period of at least 1 to 2 weeks. During this phase, antigen-specific T cells activate and clonally expand. TH1 subtypes CD4 cells activate during the sensitization phase.
DTH reactions are of two types:
- contact hypersensitivity and
- tuberculin-type hypersensitivity reactions
1. Contact hypersensitivity
Contact hypersensitivity is a type IV hypersensitivity. It occurs after sensitization with certain substances. For example, certain drugs like sulfonamides and neomycin, a component of a cosmetic or a hair dye, a metal ion such as nickel, soaps and other substances.
This reaction occurs when these substances enter the skin and combine with body proteins to become complete antigens to which a person becomes sensitized. On second exposure to the same antigen, the immune system responds by an attack of cytotoxic T cells that cause damage, mostly in the skin.
The condition shows as itching, erythema, vesicle, eczema, or necrosis of skin within 12–48 hours of the second exposure. At present the best way to avoid a DTH response to avoid the causative antigen. After the development of hypersensitivity, topical or oral corticosteroids used to suppress the destructive immune response.
2. Tuberculin-type hypersensitivity reaction
Tuberculin reaction is a typical example of delayed hypersensitivity.
Tuberculin skin test determines whether an individual has been exposed previously to Mycobacterium tuberculosis or not. In this test, a small amount of tuberculin protein is injected intradermally. If skin, at the site of injection, develop red, slightly swollen, firm lesion after 48–72 hours, it indicates a positive test.
Various other skin tests are there to detect DTH. These include many skin tests in bacterial, fungal, viral, and helminthic infections.
Symptoms
Symptoms include redness and hardness associated with pain.
Diagnosis
In Vivo, Diagnostic tests contain delayed cutaneous resistance. For example, the Montoux test and the patch test. Moreover, the tests or biopsy for delayed hypersensitivity include mitogenic responses.
TYPE V HYPERSENSITIVITY (Stimulatory Type)
Antibodies combine with antigens on the cell surface, which induces cells to proliferate and differentiate and enhances the activity of effector cells. Type V hypersensitivity reaction plays an important role in the pathogenesis of Graves’ disease, in which thyroid hormones are produced in excess quantity. Further, long-acting thyroid-stimulating antibody combines with thyroid-stimulating hormone (TSH) receptors on a thyroid cell surface. Interaction with TSH receptor produces an effect similar to the TSH, resulting in excess production and secretion of thyroid hormone, which is responsible for Graves’ disease.
REFERENCES
Textbook of microbiology and immunology by Subhash Chanda Parija, page no. 149-155.
Also, Kuby immunology, 7th edition, chapter no. 15