The female reproductive system consists of structures that produce eggs and secrete female sex hormones. They also provide a site for fertilization and enable the development and birth of a fetus.
The female reproductive system includes ovaries, fallopian tubes, uterus, vagina and vulva.
Unlike the male reproductive organs, the female reproductive organs are located mostly in the pelvic cavity. Altogether, the female reproductive system consists of the external genitalia and internal organs.
The external genitalia includes the mons pubis, labia majora, labia minora, clitoris, and structures associated with the vestibule. Although the external genitalia is often referred to as the “vagina,” the vagina is present internally and is not part of the external genitalia.
The internal organs include the vagina, cervix, uterus, fallopian tubes and ovaries. The ovaries (discussed earlier) are the primary reproductive organs in women, as well as producing female sex hormones. The vagina, uterus and fallopian tubes act as an accessory channel for the ovaries and the growing foetus.
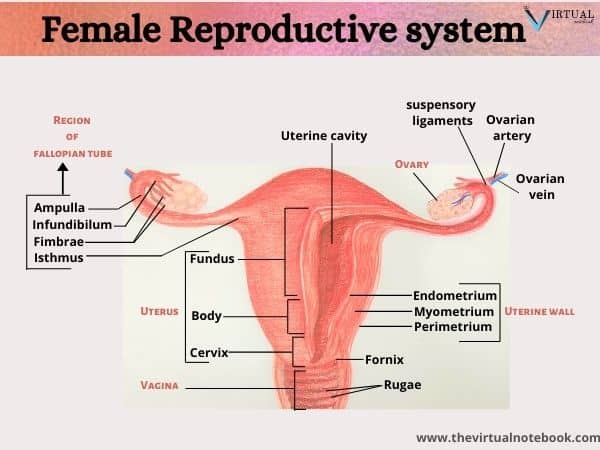
Female reproductive system labelled diagram
5 main parts of the female reproductive system
The main parts of female reproductive system are:
- Ovaries
- Fallopian tube or uterine tube
- Uterus
- Vagina
- Vulva
Among the above parts, ovaries come under primary genitalia. Fallopian tubes, uterus and vagina fall under secondary genitalia. Lastly, the vulva comes under external genitalia. Let’s discuss each part in detail. Firstly, I will talk about ovaries.
1. Ovaries
The primary organs of reproduction in the female are the ovaries. In human females, ovaries are present in a pair. They are oval in structure and are about 1.5 inches long on either side of the uterus in the pelvic cavity. Further, each ovary weighs only about 6–8 g and is about the size of a walnut.
A collection of ligaments hold the ovaries in position and attach them to the uterus. Altogether, three ligaments hold the ovaries in place and these are:
- Broad ligament: it is a large, flat ligament that attaches to the ovaries, uterine tubes, and uterus and connects them to the bony pelvis.
- Ovarian ligament: it connects the medial surface of the ovary to the uterus.
- Suspensory ligaments: finally, it connects the lateral surface of the ovary to the pelvic wall.
The ovary contains a number of small structures called ovarian follicles. Each primary ovarian follicle contains an oocyte, a potential ovum or egg cell. Surrounding the oocyte are the follicle cells, which secrete estrogen. Monthly, follicles are stimulated by two hormones, the follicle‐stimulating hormone (FSH) and LH, which stimulate the follicles to mature. The mature follicles are called the Graafian follicle.
The Graafian follicle manufacture estrogen. This estrogen is responsible for the growth of the endometrium. Every month in a menstruating woman, one or two Graafian follicle release an oocyte. This process is termed ovulation.
The remnants of a large ruptured follicle become a new structure called the corpus luteum. It produces oestrogen and progesterone. Both the hormones support the endometrium until conception takes place or the cycle starts again.
2. Fallopian tube
Other names:
uterine tube, salpinges or oviduct.
Structure
They form the first part of the female reproductive system. Like ovaries, these are also present in pair. Fallopian tubes are delicate, thin cylindrical structures approximately 8–14 cm long and extends medially from the ovary to the superior and lateral region of the uterus. They are affixed to the uterus at one end and are supported by the broad ligaments.
Further, the lateral ends of the fallopian tubes are open and comprise projections called fimbriae that drape over the ovary. These fimbriae pick up the ovum when it is discharged from the ovary. The fimbriae sweep the ovarian surface and “catch” the oocyte as the ovum has no means of self-locomotion. After that, the oocyte is carried into the fallopian tube. In the outer portion of the fallopian tube, the fertilisation of the ovum by the sperm usually occurs.
Since the ovary has no direct contact with the uterine tube, it is possible that the fimbriae will not pick up the oocyte. In such a case, it is released into the peritoneal cavity.
3. Uterus
Other name:
Womb
Position
It is present between the two ovaries in the pelvic cavity and superior to the urinary bladder. Moreover, it is anterior to the rectum and posterior to the urinary bladder.
Structure
It is a hollow, muscular organ lying in the pelvic cavity posterior and superior to the urinary bladder. It has an upside-down pear shape and is about 3 inches long by 2 inches wide by 1 inch deep. Altogether, the uterus has three sections as well as three layers:
- Fundus: it is a thick, muscular round region present above the entry of the fallopian tubes.
- Body: It is a large, main portion of the uterus, joined to the cervix by an isthmus.
- Cervix: it is a narrow, lower end of the uterus which opens into the vagina. The most inferior portion of the cervix is known as the external os. It serves as the entrance into the uterus. Glands in the mucosa of the cervical canal secrete mucus that covers the external os, acting as a protective plug.
Layers
As well as having three aspects or parts, the uterus also has three layers. These are as follows:
- Perimetrium: it is the outermost serous layer and is an extension of the parietal peritoneum. Its function is to provide support to the uterus.
- Myometrium: The middle layer is the myometrium and comprises most of the uterine wall. It is the layer that allows the uterus to stretch during pregnancy and childbirth. In addition, it contracts rhythmically during orgasm and during childbirth to expel the baby from the mother’s body and in some women, to a lesser degree, during the menstrual cycle.
- Endometrium: It is the innermost mucosal layer that lines the uterus. Structurally, the endometrium itself consists of two layers:
- Basilar layer: it is adjacent to the myometrium, vascular but very thin and is a permanent layer.
- Functional layer: On the contrary, it will regenerate and lost during each menstrual cycle. The layer grows and thickens in response to increased levels of estrogen and progesterone. Emphatically, it is the layer that provides a proper site of implantation.
4. The Vagina
The vagina is a tubular, fibromuscular structure approximately 8–10 cm in length that extends from the cervix to the exterior of the body. It is the female organ of copulation because it receives the penis (and semen) during sexual intercourse. It also provides a passageway for the delivery of an infant and for menstrual flow.
Position
It is posterior to the urinary bladder and urethra and anterior to the rectum. The upper end of the vaginal canal surrounds the external os of the cervix and produces a recess called the vaginal fornix.
Structure
The vaginal walls comprise membranous folds of tissue called the rugae. These membranes are made up of mucus‐secreting stratified squamous epithelial cells. Generally, the lumen of the vagina is quite small and its walls touch one another. However, the vagina stretches considerably during intercourse and childbirth. The vagina has no glands but remains lubricated by cervical mucus and secretions from the epithelial cells.
The epithelial cells also secrete glycogen, which resident bacteria break down to produce ATP and lactic acid. This helps maintain the acidic pH
that keeps the vagina healthy and free of infection. Usually, the walls of the vagina are moist and have a pH ranging from 3.8 to 4.2.
Hymen: In most women, the mucosa near the distal vaginal orifice forms an incomplete partition called the hymen. The thin, perforated hymen can partially surround the opening to the vaginal orifice. The hymen is very vascular and may bleed when it ruptures, which happens in about 50% of women during their first experience of sexual intercourse. However, it may also rupture from an injury or during activities such as sports.
5. Vulva
Altogether, the external genitalia is known as the vulva. They include the mons pubis, the labia, the clitoris, the vaginal and urethral openings, and glands.
The mons pubis is a pad of fat over the pubic symphysis. After puberty, the mons will cover with coarse pubic hair.
Further, Posterior to the mons is the labia majora (lateral). It is fold of hair-covered skin.
As compared to labia majora, Labia minora is thinner and more pigmented skin that extends medially to the labia majora. Although they naturally vary in shape and size from woman to woman, the labia minora serve to protect the female urethra and the entrance to the female reproductive tract.
The area between the labia minora is called the vestibule and contains the openings of the urethra and vagina.
Anterior to the vestibule is the clitoris. It is a small protruding structure that comprises erectile tissue and several nerves and blood vessels. Further, the clitoris corresponds to the corpora cavernosa of the penis and is important in the female sexual response. The region between the vagina and anus is the clinical perineum. During childbirth, some doctors will cut a straight incision, called an episiotomy through the skin and muscle of this area if a tear appears likely.
Female reproductive system functions
Function of Ovaries
The main function of ovaries are as follows:
- The primary function of the ovaries is to produce an egg or ova each month.
- Also, ovaries produce several hormones. Among these hormones are the estrogens, which include estradiol, estrone, and estriol, with estradiol being the most abundant. The ovaries also produce progesterone, inhibin, and relaxin.
Function of fallopian tubes
- They catch the oocyte when released from the ovaries.
- It is also a place where fertilization takes place.
- If fertilization occurs, fallopian tubes swept away the zygote into the uterus.
Function of uterus in female reproductive system
- It is the primary organ where implantation takes places.
- It provides both space and nourishment to the developing baby.
- Also, it expands in size during pregnancy to meet the needs of the growing baby.
Function of the vagina
- The functions of the vagina are to receive sperm from the penis during sexual intercourse.
- It provides the exit for menstrual blood flow
- Also, it functions as a birth canal at the end of pregnancy.
References
Human Anatomy and Physiology by Erin C. Amerman, Pearson chapter no. 26: Anatomy of the female reproductive system
Fundamentals of anatomy and physiology: for nursing and healthcare students, second edition, Wiley Blackwell, chapter 12: The reproductive systems
Also, Essentials of anatomy and physiology, fifth edition by Valerie C. Scanlon and Tina Sanders, chapter 20: The reproductive systems
Anatomy and physiology, Openstax, chapter 27: The reproductive systems