What is Immunity ?
Immunity is the ability of an organism to resist a particular infection or toxin by the action of specific antibodies or sensitized white blood cells. The word ‘immunity‘ came from the Latin word “
Immunity results from the combined activities of many different cells, some of which patrol the body, whereas others will concentrate in lymphoid organs, such as the bone marrow, thymus, spleen, and lymph nodes. Together, these dispersed cells and discrete organs form the body’s immune system. The main function of the immune system is to prevent or limit infections by pathogenic microorganisms, such as bacteria, viruses, parasites, and fungi.
The collective and coordinated response of the immune system to foreign substances is
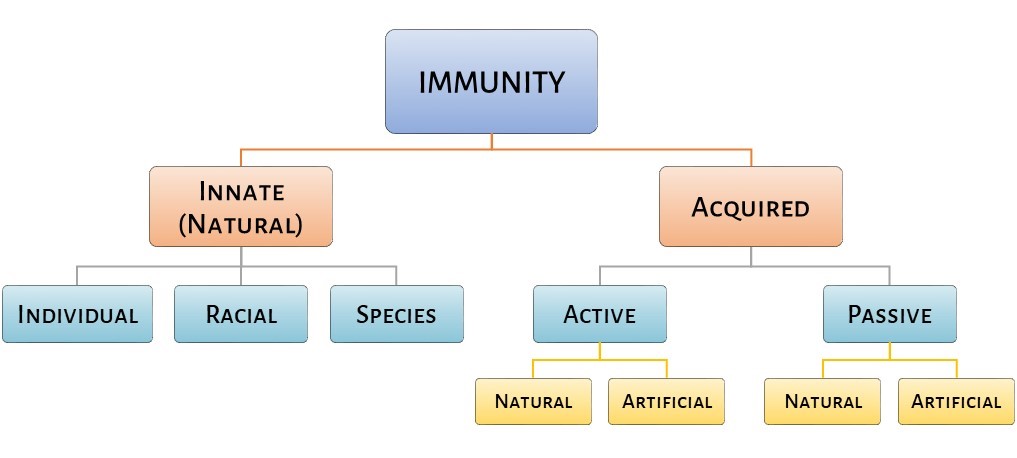
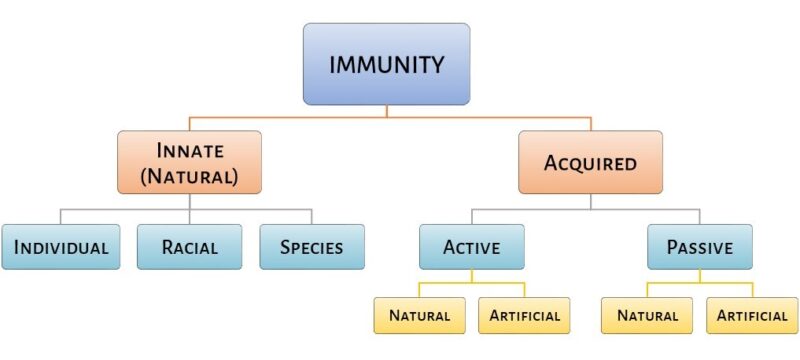
Types of immunity
Immune responses are broadly divided into two categories:
- innate (natural), or
- adaptive (or acquired) immunity.
Both types of responses depend on the ability of the body to distinguish between “self”(particles, such as proteins and other molecules, that are a part of, or produce by, our body) and “nonself” (particles that are not made by our body and are recognized as potentially harmful) materials.
First, lets start with innate immunity…
Innate immunity
Innate immunity is the resistance that an individual possesses by birth and is genetically transfer from one generation to the next. It is always general, or nonspecific. Further, it is an immediate type of immune response.
It consists of cellular and biochemical defence mechanisms that respond rapidly to infection. Also, they provide the body with the first line of defence.
The factors that may influence innate immunity
- age,
- hormonal level, and
- nutritional status of the host.
Extremes of age(either too young or too old) make an individual highly susceptible to various infections. In addition, individuals with certain hormonal disorders become increasingly susceptible to infection. For example, pregnant women are more susceptible to many infections due to higher level of steroid (hormones) during pregnancy.
The principal components of innate immunity are:
- physical and chemical barriers,
- phagocytic cells (neutrophils, macrophages), dendritic cells, and natural killer (NK) cells,
- blood proteins, including members of the complement system and other mediators of inflammation,
- cytokines that regulate and coordinate many of the activities of the cells of innate immunity.
Innate immunity may be classified as:
- individual immunity,
- racial immunity, and
- species immunity.
Individual Immunity
Individual immunity is that in which one individual of certain race or cast is resistant to an infection while other individuals of the same race or cast are susceptible to the same infection. In other words, if someone has the same racial background but experience fewer or less severe infections than other individuals of the same race, in this situation, it is known as individual immunity.
For example, children are more susceptible to diseases such as measles and chickenpox, while old individuals are susceptible to other diseases like pneumonia.
Racial immunity
Racial immunity is that in which one race is susceptible while the other race is resistant to the same infection. For example, races with sickle cell anaemia are immune to malaria. Similarly, individuals with a hereditary deficiency of glucose-6-phosphatase dehydrogenase are less susceptible to infection by Plasmodium falciparum.
Species Immunity
Species immunity denotes a total or relative resistance to a pathogen shown by all members of a particular species. For example, chickens are resistant to Bacillus anthracis, rats are resistant to Corynebacterium diphtheriae, whereas humans are susceptible to these bacteria.
Anatomic, physiological and metabolic differences between species determine species immunity. However, the exact reason for such type of immunity is not clear.
Mechanism of innate immunity
It works on two basic principles:
- Either it kills invading microbes, or
- it activates acquired immunity.
The innate immunity is primarily dependent on four types of defensive barriers:
- anatomical barriers,
- physiological barriers,
- phagocytosis, and
- inflammatory responses.
Anatomical barriers
Anatomical barriers include skin and mucous membrane. They are the most important components of innate immunity. They act as mechanical barriers and prevent the entry of microorganisms into the body.
Skin: the intact skin prevents the entry of microorganisms. For example, breaks in the skin due to scratches or wounds cause
Mucous membrane: it forms a large part of the outer covering of gastrointestinal, respiratory, genitourinary, and many other tracts of human. Saliva, tears, and mucous secretions wash away potential invading microorganisms. Hence, prevents their attachment to the initial site of infections. These secretions also contain antibacterial or antiviral substances that kill these pathogens.
Physiological Barriers
The physiological barriers that contribute to innate immunity include the following:
- Gastric acidity: very few ingested microorganisms can survive the low pH of stomach contents.
- soluble mediators
- Lysozyme: a hydrolytic enzyme found in mucosal secretions and in tears, attack on peptidoglycan layer of the bacterial cell wall.
- interferons: it comprises a group of proteins secreted by virus-infected cells. They have the ability to bind to the nearby cells and induced a generalized antiviral state.
- complement: it is a group of serum-soluble substances that when activated damage the cell membrane of the pathogenic organisms.
Phagocytosis
It is another important defence mechanism of innate immunity. Phagocytosis is a process of ingestion of extracellular particulate material by certain specialized cells, such as blood monocytes, neutrophils, and tissue macrophages.
Key steps in phagocytosis:
- bacterium attaches to pseudopodia
- ingestion of bacterium, forming phagosome
- phagosome fuses with lysosomes
- lysosomal enzymes kill and digest bacterium
- and lastly, the release of digested product from the cell.
Inflammatory responses
When the outer barriers of innate immunity, skin and other epithelial layers are damaged, the resulting innate responses to infection or tissue injury can induce a complex cascade of events known as the inflammatory response. Generally, the end result of inflammation may be the activation of a specific immune response to the invasion or clearance of the invader by components of the innate immune system.
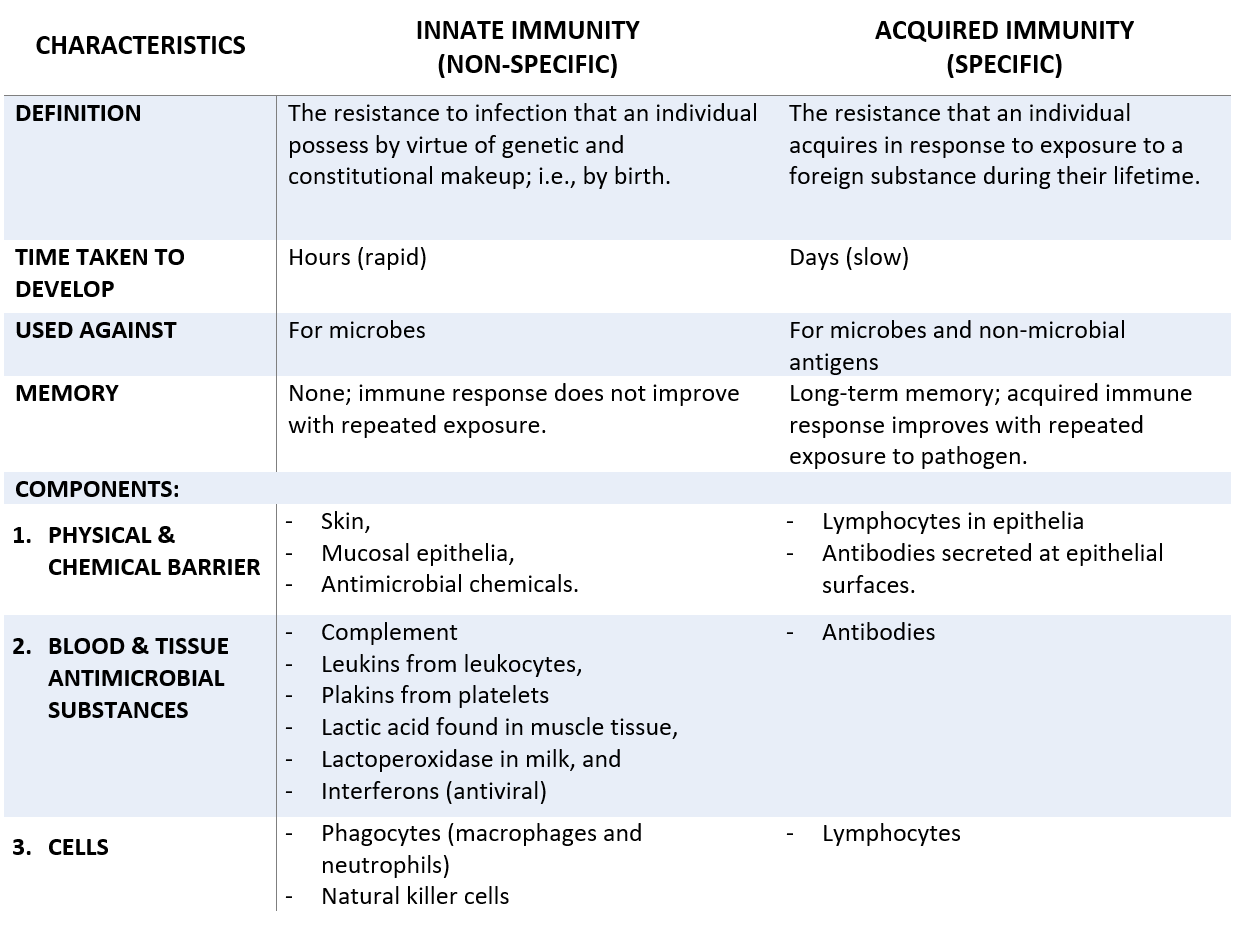
Acquired/Adaptive Immunity
It is the more specific component of immunity. It is also known as acquired immunity. Acquired immunity is highly adaptive and is capable of specifically recognizing and selectively eliminating foreign microorganisms and macromolecules, i.e., antigens.
It occurs after exposure to an agent and will mediate by antibodies as well as T lymphocytes (helper T cells and cytotoxic T cells). Moreover, it has immunologic memory and a remarkable capability of discriminating between self and nonself antigens.
Once an antigen has been recognized by the cells of the acquired immune system, the response to it is specific and can be repeated. In most cases, the acquired immune response improves with repeated exposure. The immune response to the second challenge occurs more quickly than the first, is stronger, and is often more effective in neutralizing and clearing the pathogen.
Characteristics
Adaptive or acquired immunity displays four types of characteristics attributes:
- Antigenic specificity
- diversity
- immunologic memory
- self and non-self recognition
Antigenic specificity: permits it to distinguish subtle differences among antigens. In addition, antibodies can distinguish two protein molecules that differ in only single amino acid.
Diversity: the immune system is capable of generating tremendous diversity in its recognition molecule, allowing it to recognize a variety of billions of unique structure. In general, an adaptive system can recognize a single type of organism and can differentiate among those with minor genetic differences.
Immunologic memory: adaptive immunity can store the information of all immunologic sequences when encountered by a pathogen. When there is a second encounter to the previous pathogen produces a heightened state of immune reactivity.
Self and non-self recognition: Normally, the immune system responds to only foreign antigens. It indicates that it is capable of self and non-self recognition.
Types of adaptive immunity
Adaptive or acquired immunity can be of two types:
- Active immunity
- Passive immunity
Active immunity
Active immunity is the immunity that develops after exposure to a foreign antigen. Though it takes time to develop, it is long-lasting and it is the major advantage of the active immunity. Further, it is of two types:
- natural active immunity
- artificial active immunity
Natural active immunity
It is a type of immunity that develops after natural infection. For instance, if a person will encounter a pathogen and fall ill. Now, on the second encounter with the same pathogen, he will not develop any sign of infection because he developed antibodies against the pathogen after his first encounter. Therefore, he will be immune to it. Such natural immunity is longlasting. For example, individuals suffering from smallpox become immune to the second attack of the disease.
Artificial active immunity
It is a type of immunity that develops after vaccination. Today, there are various vaccines available against a wide number of pathogens. These are live vaccines(non-virulent), killed vaccines, or vaccines containing bacterial products.
Mediators of active immunity
There are two mediators of Active immunity :
- Humoral
- cell-mediated immunity
Humoral immunity
It is mediated by antibodies present in the blood and mucosal secretions, which are produced by B lymphocytes. The antibodies will be secreted by a subset of lymphocytes known as B cells.
Humoral immunity is the principal defence mechanism against extracellular microbes and their toxins because secreted antibodies can bind to these microbes and toxins and assist in their elimination.
Cell-mediated immunity (cellular):
It is mediated by both activated TH cells and CTLs(Cytotoxic T Lymphocytes). Intracellular microbes, such as viruses and some bacteria, survive and proliferate inside phagocytes and other host cells, where they are inaccessible to circulating antibodies. Defence against such infections is a function of cell-mediated immunity.
Cytokines secreted by TH cells activate various phagocytic cells, enabling them to phagocytose and kill microorganisms. CTLs play an important role in killing virus-infected cells and
Passive Immunity
When immunity is conferred on an individual by transferring serum or lymphocytes from a specifically immunized individual, then this type of immunity is called passive immunity. Recipient of such a transfer becomes immune to the particular antigen.
Like active immunity, Passive immunity is also of two types:
- Natural, and
- artificial
Natural passive immunity
When IgG pass from mother to fetus during pregnancy, natural passive immunity develops. IgG antibody produced in mother can cross the placenta and protects fetus up to 6-month-old age.
(Read article on antibodies for information on various classes of antibodies)
Natural passive immunity will also develop by the passage of IgA from mother to newborn during breastfeeding.
Artificial passive immunity
It is induced in an individual by administration of preformed antibodies, generally in the form of antiserum, raised against an infecting agent. Administration of these antiserum makes large amounts of antibodies available in the recipient host to neutralize the action of toxins.
Immediate availability of a large number of antibodies is the main advantage of passive immunity.
Disadvantages
- the short lifespan of introduced antibodies
- possibility of hypersensitivity reaction against antibodies prepared in other animal species.
Sources and links
Textbook of microbiology and immunology by Subhash Chanda Parija, chapter 11, Immunity
Cellular ad molecular immunology, seventh edition, by Abul K. Abbas, Andrew H. Lichtman, chapter no. 1
Also, Kuby immunology, 7th edition, chapter no. 5
1 thought on “Types of Immunity: innate and adaptive”